Repairing the world
one patient at a time
Dr Daniel Meressa, former GHC Medical Coordinator (2010-2023) and St Peter’s Hospital Lead DR-TB physician and senior internist, and STREAM Trial site investigator, leading rounds on the St Peters DR-TB Ward.
Initiation of and Access to Drug Resistant TB Care in Ethiopia
GHC’s Impact 2009-2025:
1. As of 2025 February, 2953 individuals, ~20% of these children and teenagers and ~22% HIV co-infected, have been initiated on treatment for drug resistant TB care directly by the GHC/Ethiopian FMOH Collaborative Program at: St Peters Hospital in Addis Ababa (since 2009), Gondar University Hospital in Gondar, Amhara (since 2010), at Yirgalem Hospital in the Southern Nations, Nationalities, and People’s Region (SNNPR) (since 2012 (since 2012), and at Dupti Hospital in Afar Province (since 2023) as well as nutritional assistance to DR-TB patients and survivors of gender-based violence at Mekele General Hospital in Tigray (since 2023).
With the Ethiopian Ministry of Health, the GHC program also piloted outpatient initiation of treatment for DR-TB in Addis Ababa in 2010. By 2015, the highest outcomes for DR TB treatment so far achieved Africa were reported by GHC (surpassing WHO general targets) in this program with severe resource constraints and patients with advanced disease through intensive treatment of adverse effects, nutritional supplementation and adherence interventions. The non-governmental organization (NGO)–Ministry of Health collaboration, was a key feature of this success (Meressa D, Hurtado RM, Andrews JR, et al. Thorax 2015;70:1181–1188).
2. In parallel, GHC has worked closely with the Ethiopian national DR-TB program to scale-up drug resistant TB care reaching an additional +5800 individuals in the country as a whole through its work on the Ethiopian National Technical Working Committee for DR-TB , by sharing protocols for managing drug side effects, supplemental nutrition and social support and through didactic and hands-on training.
3. As the key clinical site in Ethiopia working with the STREAM Trial of the UK’s Medical Research Center and the TB UNION, GHC has been part of this game-changing work showing that a new drug regimen for DR-TB could be shortened from ~2 years to 6-9 months, providing the WHO with data in support efficacy of the newer short course regimens and use of the new TB drug bedaquiline, which GHC first acquired for Ethiopia from Janssens on a compassionate use basis for Sultan a GHC patient highlighted in the section on DR-TB in children.
All of these efforts have been in service of GHC’s vision of eradicating drug-resistant TB in Ethiopia and worldwide and providing people with access to life saving drugs for treatable but deadly infectious diseases such as TB and HIV/AIDS.
Initiating DR-TB Care in Ethiopia in 2009/ Overcoming Barriers:
When CHC first visited Ethiopia in 2008, treatment for the deadly drug resistant form of drug resistant TB (DR-TB)— also referred to as multi drug resistant-TB (MDR-TB)—was unavailable in Ethiopia, the second most populous country in Africa.
It was estimated at the time that approximately 6,000 patients a year were sick from and spreading drug resistant TB (DR-TB) in the country due to lack of access to medications. Although the country of Ethiopia had gone through a lengthy and bureaucratic process with the Green Light Committee (GLC) of the World Health Organization (WHO), which was the gate-keeper of free DR-TB drugs at the time, it was promised the drugs — 5 drug cocktails for 2 years— to treat only 45 patients. However, these drugs did not arrive and would indeed be delayed further for almost another 2 years for unclear reasons.
Seeking to share Cambodian Health Committee’s highly successful approaches to TB and HIV with programs in Africa, CHC with the support of Angelina Jolie and the Jolie-Pitt Foundation (JPF), decided to work with the Ethiopian ministry of health to implement a program to address this humanitarian crisis.
At the time, while tuberculosis (TB) itself usually takes 6 months of an all-oral treatment to achieve a cure, at the time, cure of DR-TB required 18-24 months of 5 drugs including 6-8 months of a daily painful injection, which could cause hearing loss and kidney failure. It has been estimated that untreated a person suffering with DR-TB infects at least 10 other people.
Challenges and GHC’s Responses:
Under the newly named international extension of CHC, the Global Health Committee or GHC, we sought to overcome the hurdles to starting DR-TB care in Ethiopia in partnership with the Ethiopian Ministry of Health and with the support of Dr. Tedros Adhanom who was the Minister of the Federal Ministry of Health (FMOH) of Ethiopia at the time. The flexible support of the JPF, with the generous donations of drugs from Eli Lilly &Co., Jacobus Pharmaceuticals, and the Chao Foundation and with other donors, DR-TB treatment was made possible in Ethiopia.
Ethiopian DR-TB medical team needed training in clinical management of DR-TB.
Response: CHC organized a first week-long didactic session on DR-TB patient management in Addis Ababa in the fall of 2008.
In December 2008 a team of ~10 Ethiopian doctors/nurses/TB managers came to Cambodia for a highly successful didactic and hands-on practical training experience in the management of DR-TB patients in Cambodia under the CHC team’s mentorship.
Lack of a DR-TB treatment isolation ward: no isolation ward was available as renovations of an essential isolation ward for DR-TB at St Peters Hospital, the FMOH-designated hospital for treatment of DR-TB, were a year behind without an end date in sight.
Response: With MOH support, GHC obtained permission to convert an empty ward that had been built and prepared as an isolation ward at St. Peters for a bird flu epidemic that never emerged in Ethiopia, into the first DR-TB Isolation Ward in Ethiopia This DR-TB ward went on to house the DR-TB program at St Peter’s for +2 years until the planned ward was built. And it continued for several more years to accommodate less acutely ill overflow DR-TB patients who were too numerous for the new DR-TB ward, yet needed isolation.
Lack of DR-TB drugs: in the country and no system for managing the second line DR-TB drugs was in place
Response: GHC approached Eli Lilly & Co for a donation of the most expensive drug of the 5 drug DR-TB cocktail at the time, capreomycine. Jacobus Pharamceuticals and Chao Foundations donated PASER and cycloserine respectively, with Lufthansa gifting GHC 6 free bags to be checked from the US to Addis Ababa with anyone traveling from Boston to Addis Ababa so the drugs could be hand carried. Other needed drugs were purchased by CHC in Cambodia from WHO-pre-qualified Indian companies and also hand-carried to Ethiopia. This was how the first 175 Ethiopian patients were treated In Ethiopia. Furthermore, the CHCC Pharmacist made several trips to Ethiopia to establish the second-line DR-TB Drug Pharmacy at St.
By 2012, GLC drugs and drugs purchased with grants to Ethiopia from for example the Global Fund for TB, Malaria, and AIDS and UNITAID supported drugs in the DR-TB Program, while GHC continued to support ancillary medications.
Lack of DR-TB Treatment protocols, support for Lab tests, ancillary medications, food supplementation, and social support.
Response: Based on the successful strategies for DR-TB developed in Cambodia, GHC developed protocols to manage drug side effects and outpatient follow-up and home visits. Critical was the integration of food and social support into treatment and nutritional support once patients were discharged home. As a core member of the Ethiopian national technical working group, GHC shared these strategies with the national program and the GHC collaborative programs at St Peters and at Gondar University Hospital became major training sites for the emerging national program. Specifically, GHC developed protocols for DR-TB patient intake and general management, and DR-TB drug side-effect management as well as a mobile outpatient monitoring team based on protocols developed by CHC in Cambodia.
Flexible Funding: Addressing Needs on the Ground
Flexible funding from the Jolie-Pitt Foundation allowed GHC to use funds as needed for strategic needs of the patients and programs such for lab reagents when there were stock-outs of reagents for DR-TB diagnosis and critical lab tests for side effect monitoring. Funds were also used for critical diagnostic and therapeutic procedures. As well, flexible funding allowed GHC to provide nutritious food for hospitalized DR-TB patients and food baskets for outpatients to take the multi-drug DR-TB regimens that often caused nausea and vomiting, and supported necessary transportation to the health facility or for rent for the most indigenous of the patients during their therapy.
Other very generous funders who were critical in this support through the years include the Lilly Foundation and MDR Partnership, Janssens Global Public Health, the Johnson&Johnson Foundation, Annenberg Foundation, Jeanne Sullivan, and Nancy and Steven Crown. Later, as the countrywide program developed, funds from the Global fund and other donors to the Ethiopian FMOH supported some of these needs, which were incorporated into the national program directly through national FMOH mechanisms.
Ethiopian health workers at (first and 4th left) being mentored by the CHC team (2nd and 3rd from left) in Battambang Hospital, examining a DR-TB patient in Battambang, Cambodia (December 2008)
*
Seven of the eight patients initiated on DR-TB treatment in Ethiopia in February 2009 after completion of the first 6 months of hospitalization for the intensive phase of their treatment on the repurposed ‘bird flu’ isolation ward at St Peter’s Hospital. CHC’s Dr. Sok Thim (middle row second from left), and the Ethiopian National DR-TB manager Dr. Ridwan Bushra (kneeling in first row on the right) and St Peters DR-TB nurse (in while coat) celebrated with patients who reached this critical milestone for themselves and the Ethiopian National Program.
Scenes at St Peters. Above: patients at the DR-TB Ward enjoying a music concert. Lower: A nurse checks a patient’s vital signs (left) and Dr. Rocio Hurtado, US-based GHC Medical Advisor examining a patient on rounds (right)
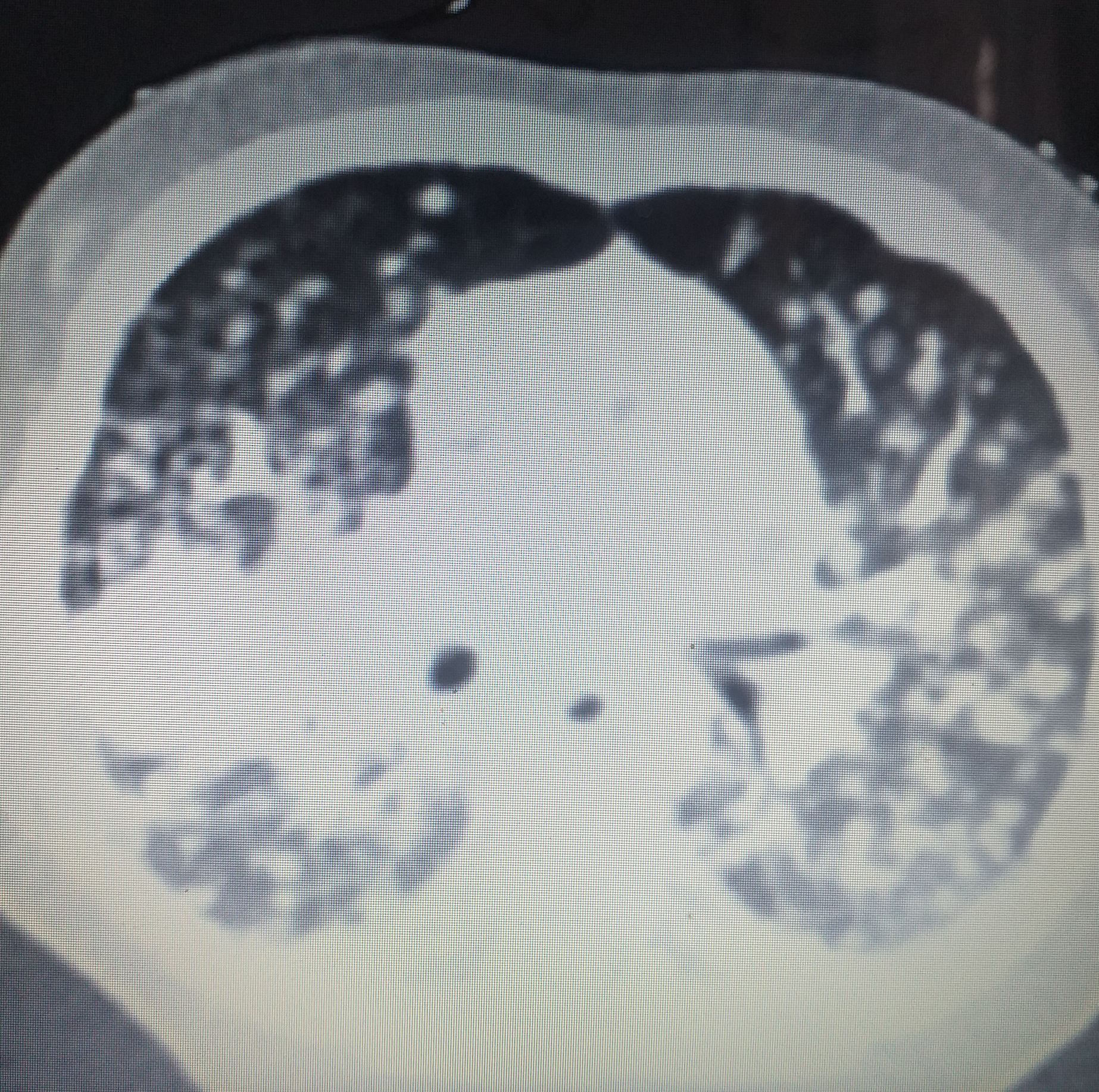
18 month old Isak on his way to DR-TB cure after 6 months of treatment at St Peters Hospital for DR-TB (left). Isak and his mother were living in an internally displaced camp due to the civil war in Tigray and he was exposed to a person who had interrupted her TB treatment in the camp. Isak was originally diagnosed with regular TB and was started on medication for regular (drug sensitive) TB for 3 months with no improvement at the internally displaced persons camp. Deteriorating clinically, he was brought to St Peters Hospital in Addis Ababa in 2022 and found to have diffuse DR-TB pneumonia (see CT scan on the right). When Isak arrived at St Peters he was in critical condition requiring oxygen, blood transfusions, and intensive care. See photos to the right of his CT scan showing diffuse DR-TB pneumonia (see asterisk showing a particularly bad region of pneumonia). Isak has done very well on treatment and at age 3 has accomplished all of his pediatric milestones such as walking and talking.
ISAK and HIS MOTHER
Mulu and her family
Mulu, a 30 year old mother of four children, was diagnosed with severe DR-TB pneumonia and malnutrition 2 months after the birth of her daughter Obse in her arms at the left. She was in respiratory failure on admission requiring oxygen and likely disseminated TB. The baby also was found to have acute malnutrition and DR-TB pneumonia. Obse developed septic shock with respiratory failure requiring oxygen shortly after they arrived at St Peter’s hospital. She survived; and, has done very well on her treatment and has met her developmental milestones, walking and doing well after 18 months of DR-TB treatment.
Her 3 year old brother Lemi (also in the picture on the left) and 8 year old sister Gadiseh (not shown) were both coughing and were evaluated by the GHC team and both were also found to have DR-TB.
Mulu and these 3 children were all successfully treated living together on the ward until they completed their treatments as their village is in a remote region. Another sibling, a 10 year old sister was also evaluated and tested negative for DR-TB and was living with her father, who also tested negative, in their home village.